Insulin and Patient Outcomes for Estrogen Receptor Positive, Her2 Negative Metastatic Breast Cancer
Metastatic breast cancer is a disease that is responsible for significant morbidity and mortality among women worldwide. In the US, there are an estimated 285,000 new cases of breast cancer each year in women and 2,700 new cases in men, with over 43,000 mortalities. Metastasis, which means the spread of cancer from the primary site to other parts of the body – typically lung, liver, bones and occasionally the brain – is the main cause of death from breast cancer. The Amelia 1 breast cancer clinical trial is enrolling now to determine the relationship between insulin and cancer in women who are being treated with Ibrance® but for whom it no longer works.
Insulin is a metabolic hormone produced by the pancreas that regulates glucose uptake in the liver, muscles, brain, adipose (fat) tissue, as well as by tumors – which also require large amounts of glucose. Insulin acts on cells via the PI3k pathway, to control GLUT4 translocation to the cell surface, permitting glucose to enter the cell. However, insulin is also a growth hormone that has known negative effects on cancer. Obesity, lack of diet/exercise, pre-diabetes, type 2 diabetes, and metabolic syndrome are commonly associated with insulin resistance. Certain cancer therapies, such as PI3k inhibitors, can also promote insulin resistance. Insulin resistance is a condition in which the body’s cells become resistant to insulin’s action, resulting in increasingly higher levels of insulin in the blood to force glucose into peripheral tissues such as adipose, liver and skeletal muscle. High levels of systemic insulin and insulin-like growth factor (IGF, a potent growth hormone linked to insulin) have been implicated in the development and progression of breast cancer.
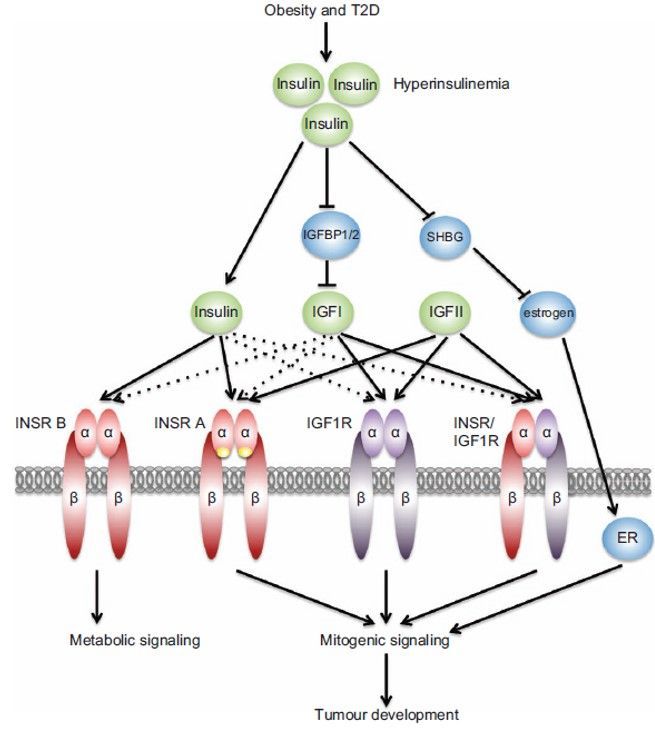
Studies have shown that insulin and IGF promote the proliferation and survival of breast cancer cells. Insulin and IGF bind to both their own receptors as well as hybrid IGF1/insulin receptors on breast cancer cells, activating downstream signaling pathways that promote cell growth and division. Aberrant expression of the fetal isoform of the insulin receptor further amplifies the growth-promoting effects of insulin as well as IGF1 and IFG2 (Gallagher EJ, LeRoith D. Hyperinsulinaemia in cancer. Nat Rev Cancer. 2020;20(11)). These pathways include the PI3K/AKT/mTOR pathway, which is frequently dysregulated in breast cancer. Activation of this pathway promotes cell survival, proliferation, and invasion, all of which are critical steps in cancer progression.
In addition to promoting cell growth and division, insulin and IGF also play a role in angiogenesis, the process by which new blood vessels grow from existing vessels, and which tumors leverage to develop their own blood supply. Angiogenesis is essential for tumor growth and metastasis. Insulin and IGF promote angiogenesis by increasing the expression of vascular endothelial growth factor (VEGF), a protein that stimulates the formation of new blood vessels.
Insulin and IGF also promote the invasion and migration of breast cancer cells. Studies have shown that insulin and IGF increase the expression of matrix metalloproteinases (MMPs), enzymes that degrade the extracellular matrix (ECM) and facilitate the migration of cancer cells. MMPs play a critical role in tumor invasion and metastasis by allowing cancer cells to break through the ECM and invade surrounding tissues.
High levels of insulin and insulin resistance have been linked to poor clinical outcomes in breast cancer patients. Several studies have shown that insulin resistance is associated with a higher risk of breast cancer recurrence and mortality. In a study of over 1,400 breast cancer patients, those with insulin resistance had a 50% higher risk of breast cancer recurrence and a 78% higher risk of mortality compared to those without insulin resistance.
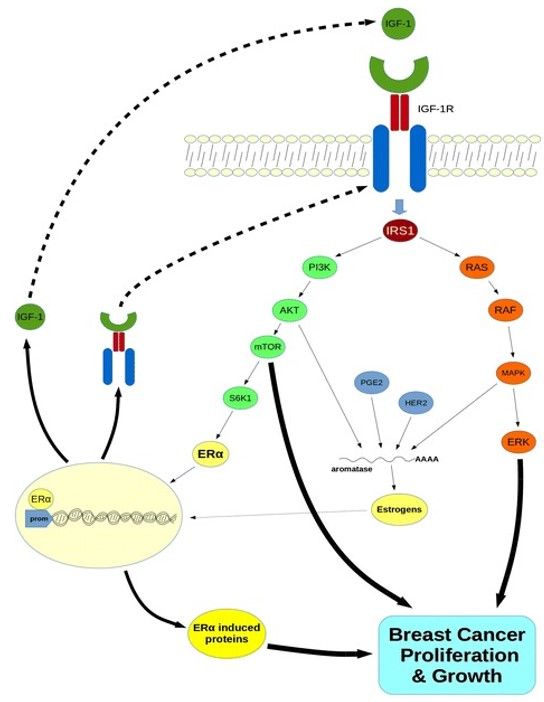
Schematic representation of the crosstalk between the IGF-1 system and estrogens in breast cancer. Binding of IGF-1 to IGF-1R triggers both PI3K/AKT/mTOR and MAPK/ERK signaling pathways, leading to enhanced breast cancer growth and proliferation. S6K1, a downstream molecule of the AKT/mTOR pathway induces phosphorylation of ERα. Activated ERα acts as transcription factor, through direct binding to promoter of target genes, consequently upregulating IGF-1, IGF-1R and other ERα-induced genes which also stimulate breast cancer progression. Prostaglandin E2 (PGE2) along with HER2 and both phosphorylated AKT and MAPK enhance aromatase activity through post-transcriptional mechanisms leading to elevated estrogen levels. Estrogens further contribute to transcriptional regulation of both IGF-1 and IGF-1R, consequently recycling the system’s signaling, enhancing growth and proliferation of breast tumors. S6K1: Ribosomal protein S6 kinase 1 protein; mTOR: mammalian target of rapamycin; HER2: human epidermal growth factor receptor 2 protein.
From: Christopoulos PF, Msaouel P, Koutsilieris M. The role of the insulin-like growth factor-1 system in breast cancer. Mol Cancer. 2015 Feb 15;14:43
Insulin resistance has also been associated with a more aggressive breast cancer phenotype, and is associated with larger tumors, higher-grade tumors, and a higher incidence of lymph node involvement compared to those patients without insulin resistance. Insulin resistance was also associated with a higher risk of developing triple-negative breast cancer, a particularly aggressive subtype of breast cancer.
In addition to insulin resistance, high levels of insulin have also been associated with poor clinical outcomes in breast cancer patients.
The Amelia-1 clinical trial is among the first therapeutic intervention specifically targeting these patients. The clinical trial is testing a new, experimental cancer treatment called evexomostat to see if it improves clinical outcomes (both safety and efficacy) when combined with the PI3k inhibitor alpelisib (Piqray®) and the estrogen receptor degrader fulvestrant (Faslodex®) in metastatic HR+/Her2- breast cancer patients. Piqray causes severe hyperglycemia and hyperinsulinemia in patients with baseline insulin resistance, obesity or metabolic syndrome, which limits its clinical benefit. The Amelia-1 trial, and its sister clinical trial for triple negative breast cancer, the Aretha-1 trial, both aim to show that reducing insulin/improving insulin resistance will positively impact the standard of care treatment, and patient outcomes.





